Chronic Venous Insufficiency With Emphasis on the Geriatric Population
Study Finds Microplastics In Blood Clots Increase Heart Attack, Stroke Risk: Here's How You Can Be Safe
Tiny bits of plastic, called microplastics (MPs), are a big problem in the environment worldwide. While we know a lot about how they affect sea creatures and oceans, we don't know much about how they affect people's health, especially their heart and blood vessels.
A recent study published in the journal eBioMedicine took blood clots from 30 patients who had strokes, heart attacks, or leg clots. They found microplastics in 80% of the blood clots, with higher amounts in sicker patients. The more microplastics there were, the worse the patients' conditions seemed to be. The most common type of microplastic found was polyethylene (PE), which was about the size of a grain of sand and had different shapes.
How Microplastics in Blood Clots Can Lead to Heart AttacksMicroplastics are tiny plastic particles less than 5 millimetres in size, often originating from the breakdown of larger plastic products or as microbeads in personal care products. These particles are pervasive in our environment, contaminating water sources, soil, and even the air we breathe. Due to their small size, microplastics can enter our bodies through ingestion, inhalation, or skin contact.
Talking about a heart attack, or myocardial infarction, it occurs when blood flow to a part of the heart is blocked, usually due to a blood clot in a coronary artery. Microplastics in blood clots can exacerbate this process in several ways:
Inflammatory ResponseMicroplastics can trigger an inflammatory response in the blood vessels, promoting the formation of atherosclerotic plaques, according to a study by the Massachusetts Medical Society. These plaques, made of cholesterol, fats, and other substances, can rupture, leading to the formation of a blood clot that blocks the artery and causes a heart attack.
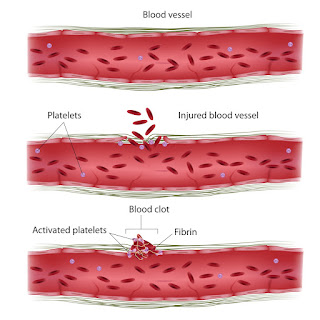
Platelet ActivationA study published in the journal Frontiers in Public Health said that microplastics can activate platelets, blood cells crucial for clot formation. Excessive platelet activation, especially in the presence of microplastics, can lead to the formation of larger and more obstructive blood clots within the arteries, increasing the risk of heart attacks.
Endothelial DysfunctionMicroplastics may impair the function of endothelial cells lining the blood vessels, according to a study published in PLOS ONE. Endothelial dysfunction is a precursor to atherosclerosis and can contribute to the development of blood clots that can trigger a heart attack.
Also Read: Columbia Study Finds 2,40,000 Nanoplastics In 1L Bottled Water: Here's How It Can Damage Your Health
As per the eBioMedicine study conducted by Chinese researchers, when microplastics enter the bloodstream, they can interact with blood components and contribute to the formation of blood clots as well, medically known as thrombosis.
Mitigating The Impact Of MicroplasticsWhile the full extent of the impact of microplastics on cardiovascular health is still being researched, there are steps individuals can take to reduce their exposure and mitigate potential risks:
The presence of microplastics in blood clots and their potential role in heart attacks highlight the need for further research and environmental actions to address plastic pollution. By raising awareness, adopting sustainable practices, and prioritising cardiovascular health, we can work towards a healthier future free from the hidden threat of microplastics.
DisclaimerAll possible measures have been taken to ensure accuracy, reliability, timeliness and authenticity of the information; however Onlymyhealth.Com does not take any liability for the same. Using any information provided by the website is solely at the viewers' discretion. In case of any medical exigencies/ persistent health issues, we advise you to seek a qualified medical practitioner before putting to use any advice/tips given by our team or any third party in form of answers/comments on the above mentioned website.
What To Know About Pulmonary Embolism?
A pulmonary embolism is a blockage in the pulmonary artery that supplies blood to the lungs. The blockage, usually caused by a blood clot, impairs oxygenation of the blood and can damage the heart. This means it can be life threatening.
The word "embolism" comes from the Greek émbolos, meaning "stopper" or "plug."
In a pulmonary embolism, the embolus forms in one part of the body and circulates throughout the blood supply. It then blocks the blood flowing through a vessel in another part of the body, namely the lungs. Blood clots often develop in the leg, which is called deep vein thrombosis (DVT).
This article lists the symptoms of pulmonary embolism and outlines its diagnosis and treatment options.
Although the exact number of those affected by pulmonary embolism or DVT is unknown, it may affect as many as 900,000 people in the United States each year.
The National Heart, Lung, and Blood Institute notes that a person may not experience any symptoms of a pulmonary embolism. Others may experience symptoms that develop within seconds to minutes or over days to weeks. The symptoms can also start mild and become more severe.
Common symptoms include:
Less common symptoms include:
Severe symptoms call for immediate emergency medical assistance. More severe cases may result in shock, loss of consciousness, cardiac arrest, and death.
Treatments for a pulmonary embolism aim to:
The main treatment option for pulmonary embolism is anticoagulation.
A doctor will prescribe anticoagulants or blood-thinning medications, such as warfarin, heparin, or direct oral anticoagulants, to stop blood clots from getting bigger and prevent new clots from forming.
They may administer an anticoagulant as soon as they suspect a pulmonary embolism before they have made a definitive diagnosis.
A person will then need to take anticoagulants for approximately 3 months or longer.
For large blood clots causing severe symptoms or complications, a doctor may prescribe an intravenous thrombolytic. However, these carry a high risk of excessive bleeding. Thrombolytics include Activase, Retavase, and Eminase.
In emergencies, a person may require surgery, such as catheter-assisted blood clot removal. A catheter-assisted blood clot removal requires a surgeon inserting a flexible tube to reach the blood clot in the lung. They can then insert a tool to break up the clot or administer medication.
A pulmonary embolism occurs when an embolus, usually a blood clot, blocks the blood flowing through an artery that feeds the lungs.
A blood clot may start in an arm or leg, known as deep vein thrombosis (DVT).
After that, it breaks free and travels through the circulatory system toward the lungs. When the embolus is too large to pass through the small vessels, it forms a blockage.
This blockage stops blood from flowing into a part of the lung. This causes the affected section of the lung to die through lack of oxygen. The blood clot can also cause pressure to build in the right side of the heart, eventually causing heart failure.
Rarely, a pulmonary embolism can result from an embolus that is formed from fat droplets, amniotic fluid, or some other particle that enters the bloodstream.
The risk factors for developing a pulmonary embolism can be genetic or acquired.
Some acquired risk factors include:
To reduce the risk of developing a blood clot or pulmonary embolism, a person can:
A person undergoing surgery should discuss a plan to prevent blood clots with a healthcare professional. They will also advise on how to prevent blood clots during the recovery period.
Those with a high risk of developing pulmonary embolism may require anticoagulant medications.
To reach a diagnosis, the doctor will look at the person's history and consider whether they are likely to have an embolism. They will carry out a physical examination. Doctors may find it challenging to make a diagnosis because other conditions have similar symptoms.
The doctor may perform the following tests:
A doctor may also perform other imaging tests so they can look at the veins and the function of the heart and lungs.
With effective and timely treatment, most people who experience a pulmonary embolism can make a full recovery. However, the condition can carry a high risk of fatality without timely intervention.
A person's outlook can also be affected depending on the underlying condition that caused the blood clot or pulmonary embolism.
A pulmonary embolism is a blockage in the pulmonary artery. The pulmonary artery supplies blood to the lungs. The blockage, which usually occurs due to a blood clot, prevents the oxygen from reaching the lungs.
Anyone experiencing symptoms of a pulmonary embolism should seek urgent medical help. This is because timely treatment and diagnosis can improve a person's outlook. Common symptoms include shortness of breath, rapid breathing, high heart rate, and pain when breathing deeply.
Treatment often involves anticoagulant medications. In severe cases, surgery may be necessary.
Mom Shares Horrifying Photo Of 20 Hidden Blood Clots Removed From Her Leg - Triggered By The Birth Of Her 'whopping' 9.5lb Baby
A30 year-old mother has shared a horrifying image of 20 giant blood clots found lurking in her leg - a gruesome side effect of birthing a 'whopping' sized baby.
Starla Ellis, 30, from Dayton, Ohio, had recently given birth to a 9lb 10.5oz newborn, following a prolonged and agonizing labor, when she began feeling 'excruciating' pain in her right leg.
Doctors at the hospital said the pain was a result of a blood clot that likely formed due to pressure on the blood vessels in her lower body.
The physicians sent her home with blood thinners - but she returned a couple of days later after her leg went totally stiff.
Scans taken revealed she in fact had scores of blood clots in her leg that would prove deadly if they weren't removed immediately.
Ms Ellis said: 'I was terrified and I didn't think I was going to make it out [of the hospital]'
Ms Ellis gave birth to her third child Amaris via emergency C-section after the baby got 'stuck'
Ms Ellis said her third child Amaris, who eventually arrived via an emergency C-section in November, got 'stuck' in her vaginal canal - which led to excessive pushing before doctors decided to take her to the OR.
After the birth, Ms Ellis went home as planned but the mother-of-three soon began to experience a 'burning ache' in her lower back, which then moved to her abdomen and into her right leg.
Ms Ellis said she first believed the pain to be her body releasing pregnancy hormones and readjusting in the weeks after giving birth to her son.
But when the pain became unbearable, she went to the hospital where she claims she was told she had one blood clot in the femoral artery in her right leg and was given blood thinners and sent home.
The 20 red blood clots laying on a piece of cloth after they were removed from Ms Ellis' right leg
Initially Ms Ellis thought the medication was working but when her leg went stiff and she couldn't bend it, she visited another hospital for a second opinion two days later.
The customer service worker claims here she underwent an ultrasound where she was told she actually had 20 clumps in her leg and they needed to be surgically removed right away.
Disturbing photos show the bulging red clots on a piece of cloth after they were removed from her right leg.
Ms Ellis claims she thought she would die and is now urging people to be persistent with their hospital referrals to ensure they get the care they need the first time round.
Ms Ellis said: 'I broke down when I saw how many blood clots were in my leg as I didn't realize it was that bad.
'Seeing a photo of all the blood clots put it into perspective of how bad it was and how close it was to me losing my life.
'Not only did the photo of the 20 blood clots shock me, it hurt my feelings that the previous doctor let me walk out of the hospital.'
According to the CDC, blood clots can be very serious and need to be treated quickly. They can lead to illness, disability and even death if not treated early.
While it remains unclear what caused the clots, Ms Ellis claims a doctor told her the blood clots could have been caused by possible C-section complications.
According to Medical News Today, there are two kinds of blood clots women may experience after giving birth.
One is clots that are passed through the vagina in the days after birth, which are from the shedding of the womb's lining and the detachment of the placenta.
Ms Ellis with her family while pregnant with her third child
Ms Ellis also said Amaris was a very 'big' baby for her size. 'I was told he was going to be a big baby and he was big for my body as I'm five foot three and he was 9lbs 10oz,' she said
The second is clots that happen inside the body's veins, which are uncommon but can be life-threatening.
This may be because pregnancy raises the pressure in the veins in your legs and pelvis, making clots more likely.
Ms Ellis also said Amaris was a very 'big' baby for her size. 'I was told he was going to be a big baby and he was big for my body as I'm five foot three and he was 9lbs 10oz,' she said.
'The pain [in my leg after the C-section] was pretty persistent and kept getting worse and I went to the emergency room.
'At this point, the pain was excruciating. I couldn't move and I had to almost crawl to the car to go to the hospital.'
Doctors ran some tests on her and discovered a blood clot in a large blood vessel in her leg. She was sent home with a blood thinner and told to follow up with her doctor in a week.
'As they discharged me I was quite concerned as I had a numbing feeling in my leg but I just ignored this as the hospital said I was good to leave.
'At first, I thought the blood thinners were working. I tried to push through as the hospital had cleared me but by that night I was back on the floor.
'My leg was completely stiff at this point and I couldn't bend it. Complete terror was going through my head and I thought I might lose my leg,' she said.
She decided to go to a different ER for a second opinion.
'I had a fever at this point and I was given pain medicine but it did not help at all as the pain was so bad.
'I was then sent up to the blood and vascular department and they ran some tests on me and did an ultrasound on my leg and they realized that the clots were a lot worse.
'I was terrified and I didn't think I was going to make it out [of the hospital].'
After being shown a photo of the 20 clots removed from her leg, she said she 'broke down' at the sight of them.
Ms Ellis said: 'You need to stay persistent with your doctor with your healthcare and they don't always seem to be as worried as you are.
'You know your body and if you feel like something is wrong you need to get it checked out.
'Make sure you follow up with your doctor as blood clots can be fatal.'


Comments
Post a Comment